Find out what's covered under the Fund's extensive Benefit Plan.
Independence Administrators (IA) are the Fund's major medical insurance provider for doctors, hospitals, and specialists. When Participants visit providers who are in-network with Independence Administrators, the Fund pays the coinsurance percentage (Gold Level 90%, Silver Level 70%) of the total IA allowance, leaving the Participant responsible for the their coinsurance portion (Gold Level 10%, Silver Level 30%). Participants are responsible for the coinsurance until they have met their out-of-pocket maximum (OOP). Once an individual or family has reached their OOP Max, the Plan will pay 100% for all further In-Network claims for the duration of the Plan Year (April 1 through March 31).
Website
Phone
1-833-242-3330
Personal Choice Coinsurance Coverage Levels
GOLD LEVEL
90/10 Coinsurance
- Active Eligibility - 600 or 1200 hours
- Out-of-Pocket Maximums $1,000 / $2,000
- Cigna Dental
- Davis Vision
SILVER LEVEL
70/30 Coinsurance
- Active Eligibility 450 or 900 Hours
- Out of Pocket Maximums $2,000 / $4,000
- No Dental Coverage
- No Vision Coverage
RETIREE HEALTH
90/10 Coinsurance
- Retire with Gold Level based on Credit System
- 1 Gold Eligibility Period = 0.50 Credit
- 1 Silver Eligibility Period = 0.25
- Maximum of 1 Credit in a Plan Year
Prescription Coverage is the same for both Gold and Silver Levels
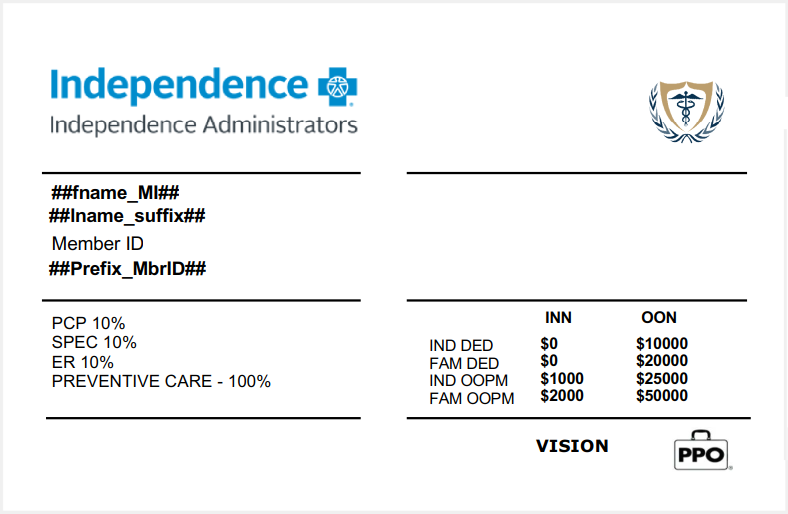
Major Medical Insurance Card
Use this card when visiting any in-network doctor, hospital, specialist. If you need a replacement card please call 1-833-242-3330.
Addtional Benefits Covered Through Independence Administrators
Lab Work is covered 100% if processed through LabCorp. If processed through an in-network lab, doctor or hospital, it would be covered under your respective coinsurance coverage level (Gold Level 90/10, Silver Level 70/30).
Show your Independence Administrators insurance card at any in-network chiropractor.
Learn more about the Chiropractic Treatment Benefit.
Use the Independence Administrators insurance card at any in-network acupuncture treatment facility.
Air Ambulance is covered through Independence Administrators.